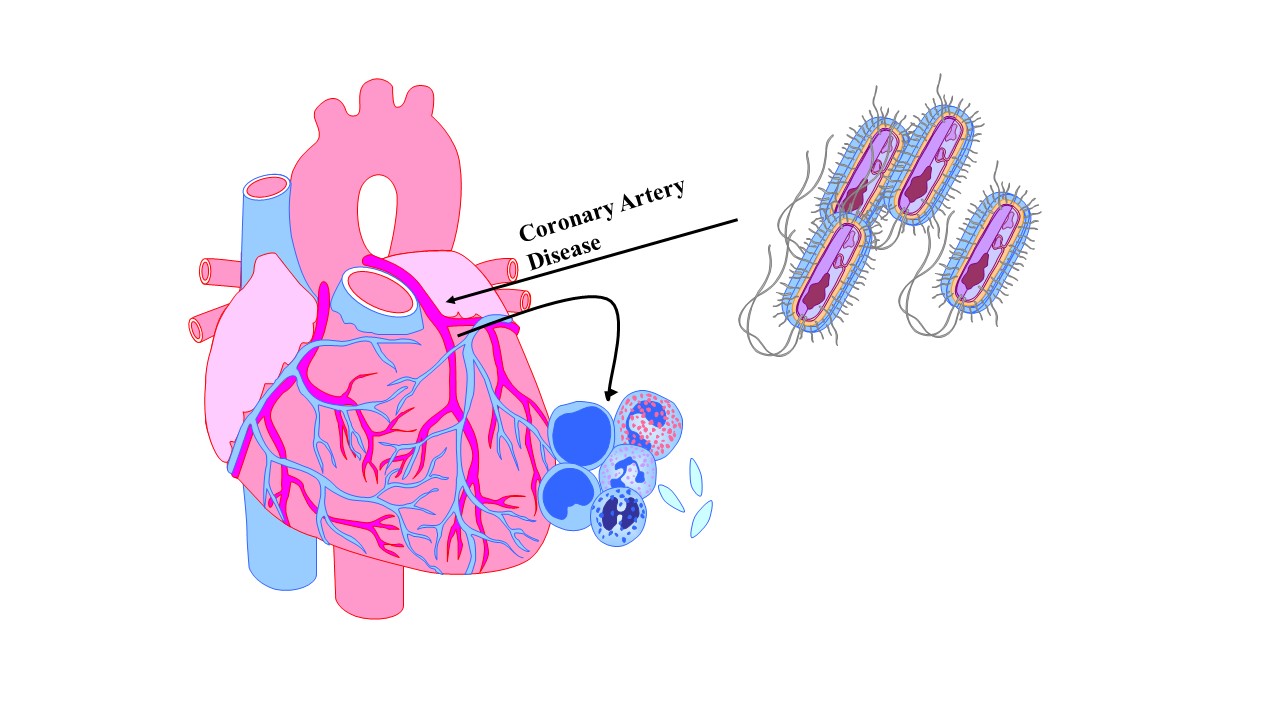
Porphyromonas gingivalis Infection is Associated with Increased Vascular Inflammation in Patients with and Without Coronary Artery Disease
DOI:
https://doi.org/10.13052/ijts2246-8765.2024.026Keywords:
Periodontal disease, vascular inflammation, porphyromonas gingivalis, biomarkers, coronary artery diseaseAbstract
Vascular inflammation is a critical measure of risk for major adverse cardiac events in patients with and without known coronary artery disease. It is recognized that patients with poor oral hygiene tend to have an increased prevalence of coronary artery disease and myocardial infarction. Porphyromonas gingivalis (PG) is the keystone pathogen leading to periodontal disease. Despite evidence suggesting a link between active PG infection and coronary artery disease, there is limited data investigating whether PG can contribute to increased markers of vascular inflammation in patients with coronary artery disease. In this study, we studied 112 consecutive patients who presented at a community preventive cardiology clinic who consented to be assessed for the presence of PG. Subjects were enrolled in a mouth along assessment with measures of vascular inflammation, which was part of their routine clinical care. The average age of patients was 70.4 ± 8.5 years with 48.6% of the patients positive for PG and 20.5% with a history of coronary artery disease (CAD). The distribution of PG positivity was 48.3% and 34.8% in patients without and with a history of CAD, respectively. Patients with CAD have significantly greater levels of high sensitivity C-reactive protein (hsCRP_ (1.3 ± 0.3 vs. 3.2 ± 1.1 mg/dL, p = 0.04) and MPO (245.1 ± 19.4 vs. 371.4 ± 39.1 pmol/L, p = 0.003). Patients without a history of CAD, only Myeloperoxidase (MPO) was significantly increased. Statin use was significantly greater in those patients with a history of CAD. Interestingly, statin use tended to be greater in PG+ patients (71% vs. 62%) regardless of CAD status. The data from this early study demonstrate a link between active PG infection and increase in markers of vascular inflammation, especially in patients with established CAD. The findings suggest PG as a marker of cardiovascular risk, especially in patients with residual inflammatory risk.
Downloads
References
Ridker PM, Bhatt DL, Pradhan AD, Glynn RJ, MacFadyen JG, Nissen SE, et al. Inflammation and cholesterol as predictors of cardiovascular events among patients receiving statin therapy: a collaborative analysis of three randomised trials. Lancet. 2023;401:1293–301.
Penn MS, MacRae C, Goldfaden RF, Choksi RR, Smith S, Wrenn D, et al. Association of chronic neutrophil activation with risk of mortality. PloS one. 2023;18:e0288712.
Mohammadnia N, Opstal TSJ, El Messaoudi S, Bax WA, Cornel JH. An Update on Inflammation in Atherosclerosis: How to Effectively Treat Residual Risk. Clinical therapeutics. 2023;45:1055–9.
Durante A, Bronzato S. The increased cardiovascular risk in patients affected by autoimmune diseases: review of the various manifestations. J Clin Med Res. 2015;7:379–84.
Chakaroun RM, Olsson LM, Backhed F. The potential of tailoring the gut microbiome to prevent and treat cardiometabolic disease. Nature Rev Cardiology. 2023;20:217–35.
Ramirez JH, Parra B, Gutierrez S, Arce RM, Jaramillo A, Ariza Y, et al. Biomarkers of cardiovascular disease are increased in untreated chronic periodontitis: a case control study. Aust Dent J. 2014;59:29–36.
Rao A, Kumar BK. Role of periodontal pathogens in atherosclerotic plaque development and progression: An overview. Acta Microbiol Immunol Hung. 2023;70:272–7.
Nara PL, Sindelar D, Penn MS, Potempa J, Griffin WST. Porphyromonas gingivalis Outer Membrane Vesicles as the Major Driver of and Explanation for Neuropathogenesis, the Cholinergic Hypothesis, Iron Dyshomeostasis, and Salivary Lactoferrin in Alzheimer’s Disease. J Alzheimers Dis. 2021;82:1417–50.
Gao S, Zhang Z, Sun K, Li MX, Qi YJ. Upper gastrointestinal tract microbiota with oral origin in relation to oesophageal squamous cell carcinoma. Annals Med. 2023;55:2295401.
Sabbagh MN, Decourt B. COR388 (atuzaginstat): an investigational gingipain inhibitor for the treatment of Alzheimer disease. Expert Opin Investig Drugs. 2022;31:987–93.
Xiao L, Huang L, Zhou X, Zhao D, Wang Y, Min H, et al. Corrigendum: Experimental Periodontitis Deteriorated Atherosclerosis Associated With Trimethylamine N-Oxide Metabolism in Mice. Front Cell Infect Microbiol. 2022;12:919013.
Hernández-Ruiz P, Escalona Montaño AR, Amezcua-Guerra LM, González-Pacheco H, Niccolai E, Amedei A, et al. Potential Association of the Oral Microbiome with Trimethylamine N-Oxide Quantification in Mexican Patients with Myocardial Infarction. Mediators of inflammation. 2024;2024:3985731.