Chrono-Nutrition: Understanding the Interplay Between Circadian Rhythms and Personalized Nutrition
DOI:
https://doi.org/10.13052/ijts2246-8765.2024.035Keywords:
Chronobiology, nutrition, microbiome, circadian rhythmAbstract
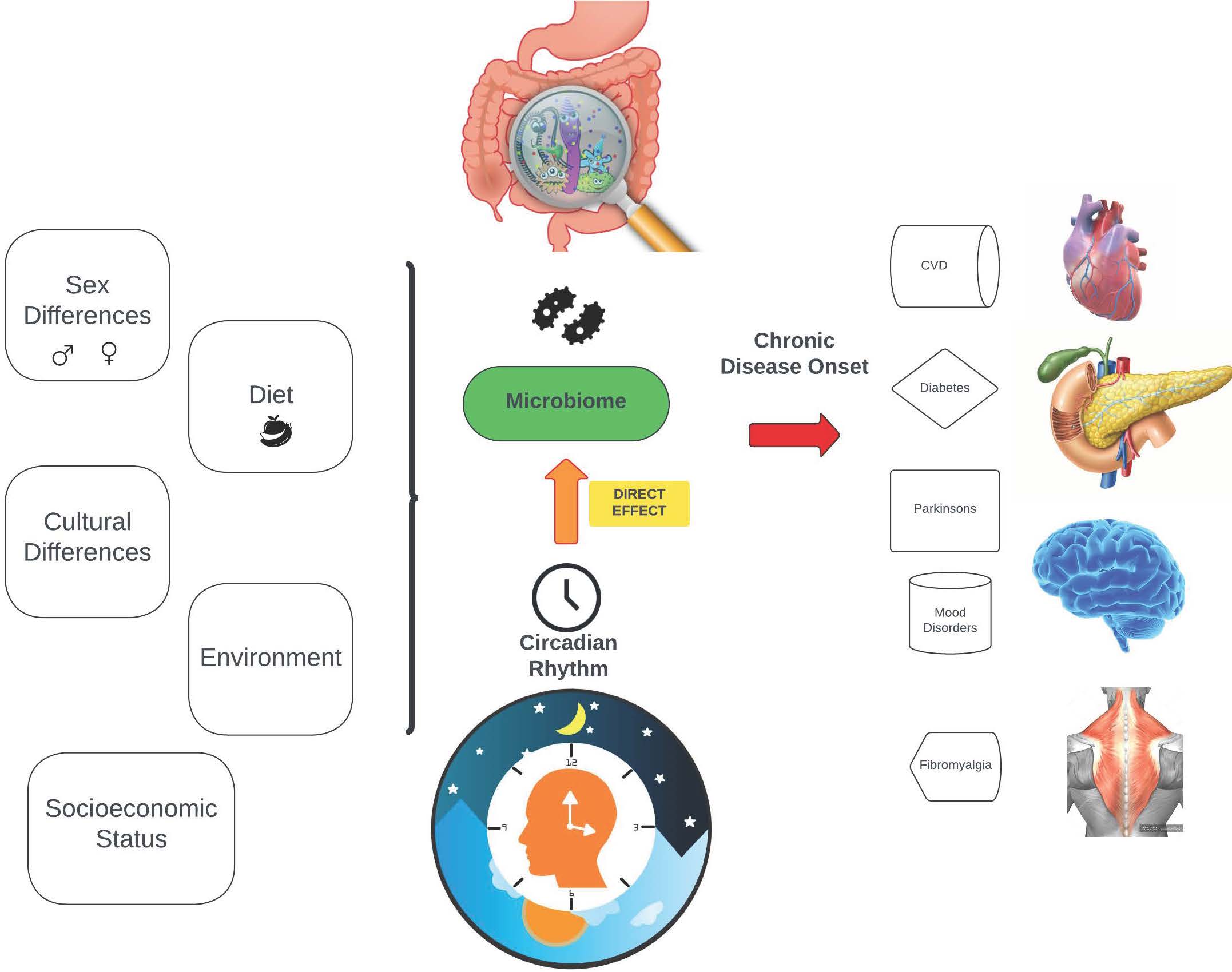
Chrono-nutrition, a concept emerging from the integration of chronobiology and nutrition sciences, investigates the timing of food intake in alignment with the body’s circadian rhythms. This interplay between dietary patterns and biological rhythms has garnered significant attention in recent years due to its potential implications for health and disease. In this comprehensive review, we explore the key findings from studies in the last decade on chrono-nutrition, focusing on its role in cardiovascular health, diabetes management, glucose metabolism, and the influence of sex, socioeconomic factors, and cultural diversity. The intricate dance between the molecular circadian clock and the gut microbiome is a fascinating area of study in modern biology. Both systems are integral to the regulation of metabolic processes, responding to dietary inputs and environmental cues to optimize the host’s adaptability and survival. This review delves into the dynamic interplay between circadian rhythms and the gut microbiome, exploring their mutual influence and the implications for human health.
Downloads
References
Al Abdi, T., Andreou, E., Papageorgiou, A., Heraclides, A., and Philippou, E. 2020. Personality, Chrono-nutrition and Cardiometabolic Health: A Narrative Review of the Evidence. Advances in nutrition (Bethesda, Md.). 11(5), 1201–1210. https:/doi.org/10.1093/advances/nmaa051.
Almoosawi, S., Vingeliene, S., Gachon, F., Voortman, T., Palla, L., Johnston, J. D., Van Dam, R. M., Darimont, C., and Karagounis, L. G. 2019. Chronotype: Implications for Epidemiologic Studies on Chrono-Nutrition and Cardiometabolic Health. Advances in nutrition (Bethesda, Md.). 10(1), 30–42. https:/doi.org/10.1093/advances/nmy070.
Rana, S., Prabhu, S. D., and Young, M. E. Chronobiological Influence Over Cardiovascular Function: The Good, the Bad, and the Ugly. 2020. Circulation research. 126(2), 258–279. https:/doi.org/10.1161/CIRCRESAHA.119.313349.
Hudec, M., Dankova, P., Solc, R., Bettazova, N., and Cerna, M. 2020. Epigenetic Regulation of Circadian Rhythm and Its Possible Role in Diabetes Mellitus. International journal of molecular sciences. 21(8), 3005. https:/doi.org/10.3390/ijms21083005.
Moreno-Cortés, M. L., Meza-Alvarado, J. E., García-Mena, J., and Hernández-Rodríguez, A. 2024. Chronodisruption and Gut Microbiota: Triggering Glycemic Imbalance in People with Type 2 Diabetes. Nutrients. 16(5), 616. https:/doi.org/10.3390/nu16050616.
Maury E. 2019. Off the Clock: From Circadian Disruption to Metabolic Disease. International journal of molecular sciences. 20(7), 1597. https:/doi.org/10.3390/ijms20071597.
Pot G. K. 2018. Sleep and dietary habits in the urban environment: the role of chrono-nutrition. The Proceedings of the Nutrition Society. 77(3), 189–198. https:/doi.org/10.1017/S0029665117003974.
Franzago, M., Alessandrelli, E., Notarangelo, S., Stuppia, L., and Vitacolonna, E. 2023. Chrono-Nutrition: Circadian Rhythm and Personalized Nutrition. International journal of molecular sciences. 24(3), 2571. https:/doi.org/10.3390/ijms24032571.
Henry, C. J., Kaur, B., and Quek, R. Y. C. 2020. Chrononutrition in the management of diabetes. Nutrition and diabetes. 10(1), 6. https:/doi.org/10.1038/s41387-020-0109-6.
Senesi, P., Ferrulli, A., Luzi, L., and Terruzzi, I. 2022. Chrono-communication and cardiometabolic health: The intrinsic relationship and therapeutic nutritional promises. Frontiers in endocrinology. 13, 975509. https:/doi.org/10.3389/fendo.2022.975509.
McHill, A. W., Hull, J. T., and Klerman, E. B. 2022. Chronic Circadian Disruption and Sleep Restriction Influence Subjective Hunger, Appetite, and Food Preference. Nutrients. 14(9), 1800. https:/doi.org/10.3390/nu14091800.
Bohmke, N. J., Dixon, D. L., and Kirkman, D. L. 2024. Chrono-nutrition for hypertension. Diabetes/metabolism research and reviews. 40(1), e3760. https:/doi.org/10.1002/dmrr.3760.
Vallée, A., Lecarpentier, Y., Guillevin, R., and Vallée, J. N. 2020. Circadian rhythms, Neuroinflammation and Oxidative Stress in the Story of Parkinson’s Disease. Cells. 9(2), 314. https:/doi.org/10.3390/cells9020314.
Wilson, J. E., Blizzard, L., Gall, S. L., Magnussen, C. G., Oddy, W. H., Dwyer, T., Sanderson, K., Venn, A. J., and Smith, K. J. 2020. An eating pattern characterised by skipped or delayed breakfast is associated with mood disorders among an Australian adult cohort. Psychological medicine. 50(16), 2711–2721. https:/doi.org/10.1017/S0033291719002800.
Zhang, R., Cai, X., Lin, C., Yang, W., Lv, F., Wu, J., and Ji, L. 2022. The association between metabolic parameters and evening chronotype and social jetlag in non-shift workers: A meta-analysis. Frontiers in endocrinology. 13, 1008820. https:/doi.org/10.3389/fendo.2022.1008820.
Gutierrez Lopez, D. E., Lashinger, L. M., Weinstock, G. M., and Bray, M. S. 2021. Circadian rhythms and the gut microbiome synchronize the host’s metabolic response to diet. Cell metabolism. 33(5), 873–887. https:/doi.org/10.1016/j.cmet.2021.03.015.
Matenchuk, B. A., Mandhane, P. J., and Kozyrskyj, A. L. 2020. Sleep, circadian rhythm, and gut microbiota. Sleep medicine reviews. 53, 101340. https:/doi.org/10.1016/j.smrv.2020.101340.
Yan, R., Chung, S. Y., and Xin, Z. 202. Maintain host health with time-restricted eating and phytochemicals: A review based on gut microbiome and circadian rhythm. Trends in Food Science and Technology, 108, 258–268. Maintain host health with time-restricted eating and phytochemicals: A review based on gut microbiome and circadian rhythm – ScienceDirect
Fawad, J. A., Luzader, D. H., Hanson, G. F., Moutinho, T. J., Jr, McKinney, C. A., Mitchell, P. G., Brown-Steinke, K., Kumar, A., Park, M., Lee, S., Bolick, D. T., Medlock, G. L., Zhao, J. Y., Rosselot, A. E., Chou, C. J., Eshleman, E. M., Alenghat, T., Hong, C. I., Papin, J. A., and Moore, S. R. 2022. Histone Deacetylase Inhibition by Gut Microbe-Generated Short-Chain Fatty Acids Entrains Intestinal Epithelial Circadian Rhythms. Gastroenterology. 163(5), 1377–1390.e11. https:/doi.org/10.1053/j.gastro.2022.07.051.
Gumz, M. L., Shimbo, D., Abdalla, M., Balijepalli, R. C., Benedict, C., Chen, Y., Earnest, D. J., Gamble, K. L., Garrison, S. R., Gong, M. C., Hogenesch, J. B., Hong, Y., Ivy, J. R., Joe, B., Laposky, A. D., Liang, M., MacLaughlin, E. J., Martino, T. A., Pollock, D. M., Redline, S., …Oh, Y. S. 2023. Toward Precision Medicine: Circadian Rhythm of Blood Pressure and Chronotherapy for Hypertension – 2021 NHLBI Workshop Report. Hypertension (Dallas, Tex. : 1979). 80(3), 503–522. https:/doi.org/10.1161/HYPERTENSIONAHA.122.19372.
Flanagan, A., Bechtold, D. A., Pot, G. K., and Johnston, J. D. 2021. Chrono-nutrition: From molecular and neuronal mechanisms to human epidemiology and timed feeding patterns. Journal of neurochemistry. 157(1), 53–72. https:/doi.org/10.1111/jnc.15246.
Bermingham, K. M., Stensrud, S., Asnicar, F., Valdes, A. M., Franks, P. W., Wolf, J., Hadjigeorgiou, G., Davies, R., Spector, T. D., Segata, N., Berry, S. E., and Hall, W. L. 2023. Exploring the relationship between social jetlag with gut microbial composition, diet and cardiometabolic health, in the ZOE PREDICT 1 cohort. European journal of nutrition. 62(8), 3135–3147. https:/doi.org/10.1007/s00394-023-03204-x.
Dashti, H. S., Gómez-Abellán, P., Qian, J., Esteban, A., Morales, E., Scheer, F. A. J. L., and Garaulet, M. 2021. Late eating is associated with cardiometabolic risk traits, obesogenic behaviors, and impaired weight loss. The American journal of clinical nutrition. 113(1), 154–161. https:/doi.org/10.1093/ajcn/nqaa264.
Arab, A., Karimi, E., Garaulet, M., and Scheer, F. A. J. L. 2023. Social jetlag and dietary intake: A systematic review. Sleep medicine reviews. 71, 101820. https:/doi.org/10.1016/j.smrv.2023.101820.
Moon, S., Kang, J., Kim, S. H., Chung, H. S., Kim, Y. J., Yu, J. M., Cho, S. T., Oh, C. M., and Kim, T. 2020. Beneficial Effects of Time-Restricted Eating on Metabolic Diseases: A Systemic Review and Meta-Analysis. Nutrients. 12(5), 1267. https:/doi.org/10.3390/nu12051267.
Zheng, D., Ratiner, K., and Elinav, E. 2020. Circadian Influences of Diet on the Microbiome and Immunity. Trends in immunology. 41(6), 512–530. https:/doi.org/10.1016/j.it.2020.04.005.
Hawley, J. A., Sassone-Corsi, P., and Zierath, J. R. 2020. Chrono-nutrition for the prevention and treatment of obesity and type 2 diabetes: from mice to men. Diabetologia. 63(11), 2253–2259. https:/doi.org/10.1007/s00125-020-05238-w.
Adafer, R., Messaadi, W., Meddahi, M., Patey, A., Haderbache, A., Bayen, S., and Messaadi, N. 2020. Food Timing, Circadian Rhythm and Chrononutrition: A Systematic Review of Time-Restricted Eating’s Effects on Human Health. Nutrients. 12(12), 3770. https:/doi.org/10.3390/nu12123770.
Stenvers, D. J., Scheer, F. A. J. L., Schrauwen, P., la Fleur, S. E., and Kalsbeek, A. 2019. Circadian clocks and insulin resistance. Nature reviews. Endocrinology. 15(2), 75–89. https:/doi.org/10.1038/s41574-018-0122-1.
Levine, B., and Kroemer, G. 2019. Biological Functions of Autophagy Genes: A Disease Perspective. Cell. 176(1-2), 11–42. https:/doi.org/10.1016/j.cell.2018.09.048.
Wang, Z. H., Wu, W., Kang, S. S., Liu, X., Wu, Z., Peng, J., Yu, S. P., Manfredsson, F. P., Sandoval, I. M., Liu, X., Wang, J. Z., and Ye, K. 2018. BDNF inhibits neurodegenerative disease-associated asparaginyl endopeptidase activity via phosphorylation by AKT. JCI insight. 3(16), e99007. https:/doi.org/10.1172/jci.insight.99007.
Aoyama, S., and Shibata, S. 2020. Time-of-Day-Dependent Physiological Responses to Meal and Exercise. Frontiers in nutrition. 7, 18. https:/doi.org/10.3389/fnut.2020.00018.
Mason, I. C., Qian, J., Adler, G. K., and Scheer, F. A. J. L. 2020. Impact of circadian disruption on glucose metabolism: implications for type 2 diabetes. Diabetologia. 63(3), 462–472. https:/doi.org/10.1007/s00125-019-05059-6.
Poggiogalle, E., Jamshed, H., and Peterson, C. M. 2018. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism: clinical and experimental. 84, 11–27. https:/doi.org/10.1016/j.metabol.2017.11.017.
Peng, F., Li, X., Xiao, F., Zhao, R., and Sun, Z. 2022. Circadian clock, diurnal glucose metabolic rhythm, and dawn phenomenon. Trends in neurosciences. 45(6), 471–482. https:/doi.org/10.1016/j.tins.2022.03.010.
Yang, Y., and Zhang, J. 2020. Bile acid metabolism and circadian rhythms. American journal of physiology. Gastrointestinal and liver physiology. 319(5), G549–G563. https:/doi.org/10.1152/ajpgi.00152.2020.
Carasso, S., Fishman, B., Lask, L. S., Shochat, T., Geva-Zatorsky, N., and Tauber, E. 2021. Metagenomic analysis reveals the signature of gut microbiota associated with human chronotypes. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 35(11), e22011. https:/doi.org/10.1096/fj.202100857RR.
Carrasco-Querol, N., Cabricano-Canga, L., Bueno Hernández, N., Gonçalves, A. Q., Caballol Angelats, R., Pozo Ariza, M., Martín-Borràs, C., Montesó-Curto, P., Castro Blanco, E., Dalmau Llorca, M. R., and Aguilar Martín, C. 2024. Nutrition and Chronobiology as Key Components of Multidisciplinary Therapeutic Interventions for Fibromyalgia and Associated Chronic Fatigue Syndrome: A Narrative and Critical Review. Nutrients. 16(2), 182. https:/doi.org/10.3390/nu16020182.
Bjørklund G, Dadar M, Chirumbolo S, Aaseth J. 2018 Jul. Fibromyalgia and nutrition: Therapeutic possibilities? Biomed Pharmacother. 103:531-538. doi: 10.1016/j.biopha.2018.04.056. Epub 2018 Apr 24. PMID: 29677539.
Codoñer-Franch, P., Gombert, M., Martínez-Raga, J., and Cenit, M. C. 2023. Circadian Disruption and Mental Health: The Chronotherapeutic Potential of Microbiome-Based and Dietary Strategies. International journal of molecular sciences. 24(8), 7579. https:/doi.org/10.3390/ijms24087579.
Lotti, S., Dinu, M., Colombini, B., Amedei, A., and Sofi, F. 2023. Circadian rhythms, gut microbiota, and diet: Possible implications for health. Nutrition, metabolism, and cardiovascular diseases : NMCD. 33(8), 1490–1500. https:/doi.org/10.1016/j.numecd.2023.05.009.
Frazier, K., and Chang, E. B. 2020. Intersection of the Gut Microbiome and Circadian Rhythms in Metabolism. Trends in endocrinology and metabolism: TEM. 31(1), 25–36. https:/doi.org/10.1016/j.tem.2019.08.013.
Litichevskiy, L., and Thaiss, C. A. 2022. The Oscillating Gut Microbiome and Its Effects on Host Circadian Biology. Annual review of nutrition. 42, 145–164. https:/doi.org/10.1146/annurev-nutr-062320-111321.
Butler, T. D., and Gibbs, J. E. 2020. Circadian Host-Microbiome Interactions in Immunity. Frontiers in immunology. 11, 1783. https:/doi.org/10.3389/fimmu.2020.01783.
Jamshed, H., Beyl, R. A., Della Manna, D. L., Yang, E. S., Ravussin, E., and Peterson, C. M. 2019. Early Time-Restricted Feeding Improves 24-Hour Glucose Levels and Affects Markers of the Circadian Clock, Aging, and Autophagy in Humans. Nutrients. 11(6), 1234. https:/doi.org/10.3390/nu11061234.
Roth, J. R., Varshney, S., de Moraes, R. C. M., and Melkani, G. C. 2023. Circadian-mediated regulation of cardiometabolic disorders and aging with time-restricted feeding. Obesity (Silver Spring, Md.). 31 Suppl 1(Suppl 1), 40–49. https:/doi.org/10.1002/oby.23664.
Leng, Y., Musiek, E. S., Hu, K., Cappuccio, F. P., and Yaffe, K. 2019. Association between circadian rhythms and neurodegenerative diseases. The Lancet. Neurology. 18(3), 307–318. https:/doi.org/10.1016/S1474-4422(18)30461-7.
Mattis, J., and Sehgal, A. 2016. Circadian Rhythms, Sleep, and Disorders of Aging. Trends in endocrinology and metabolism: TEM. 27(4), 192–203. https:/doi.org/10.1016/j.tem.2016.02.003.
Prudon, B., Duncan, G. W., Khoo, T. K., Yarnall, A. J., and Anderson, K. N. 2014. Primary sleep disorder prevalence in patients with newly diagnosed Parkinson’s disease. Movement disorders : official journal of the Movement Disorder Society. 29(2), 259–262. https:/doi.org/10.1002/mds.25730.
De Lazzari, F., Bisaglia, M., Zordan, M. A., and Sandrelli, F. 2018. Circadian Rhythm Abnormalities in Parkinson’s Disease from Humans to Flies and Back. International journal of molecular sciences. 19(12), 3911. https:/doi.org/10.3390/ijms19123911.
Fifel, K., and De Boer, T.2021. The circadian system in Parkinson’s disease, multiple system atrophy, and progressive supranuclear palsy. Handbook of clinical neurology. 179, 301–313. https:/doi.org/10.1016/B978-0-12-819975-6.00019-4.
Kunz, D., Oster, H., Rawashdeh, O., Neumann, W. J., Münte, T., and Berg, D. 2023. Sleep and circadian rhythms in α
-synucleinopathies-Perspectives for disease modification. Acta physiologica (Oxford, England). 238(1), e13966. https:/doi.org/10.1111/apha.13966.
Simpson, C. A., Diaz-Arteche, C., Eliby, D., Schwartz, O. S., Simmons, J. G., and Cowan, C. S. M. 2021. The gut microbiota in anxiety and depression – A systematic review. Clinical psychology review. 83, 101943. https:/doi.org/10.1016/j.cpr.2020.101943.
Yang, D. F., Huang, W. C., Wu, C. W., Huang, C. Y., Yang, Y. S. H., and Tung, Y. T. 2023. Acute sleep deprivation exacerbates systemic inflammation and psychiatry disorders through gut microbiota dysbiosis and disruption of circadian rhythms. Microbiological research. 268, 127292. https:/doi.org/10.1016/j.micres.2022.127292.
Logan, R. W., and McClung, C. A. 2019. Rhythms of life: circadian disruption and brain disorders across the lifespan. Nature reviews. Neuroscience. 20(1), 49–65. https:/doi.org/10.1038/s41583-018-0088-y.
Walton, J. C., Bumgarner, J. R., and Nelson, R. J. 2022. Sex Differences in Circadian Rhythms. Cold Spring Harbor perspectives in biology. 14(7), a039107. https:/doi.org/10.1101/cshperspect.a039107.
Joye, D. A. M., and Evans, J. A. 2022. Sex differences in daily timekeeping and circadian clock circuits. Seminars in cell and developmental biology. 126, 45–55. https:/doi.org/10.1016/j.semcdb.2021.04.026.
Logan, R. W., Xue, X., Ketchesin, K. D., Hoffman, G., Roussos, P., Tseng, G., McClung, C. A., and Seney, M. L. 2022. Sex Differences in Molecular Rhythms in the Human Cortex. Biological psychiatry. 91(1), 152–162. https:/doi.org/10.1016/j.biopsych.2021.03.005.
Škrlec, I., Talapko, J., Juzbašić, M., and Steiner, R. 2021. Sex Differences in Circadian Clock Genes and Myocardial Infarction Susceptibility. Journal of cardiovascular development and disease. 8(5), 53. https:/doi.org/10.3390/jcdd8050053.