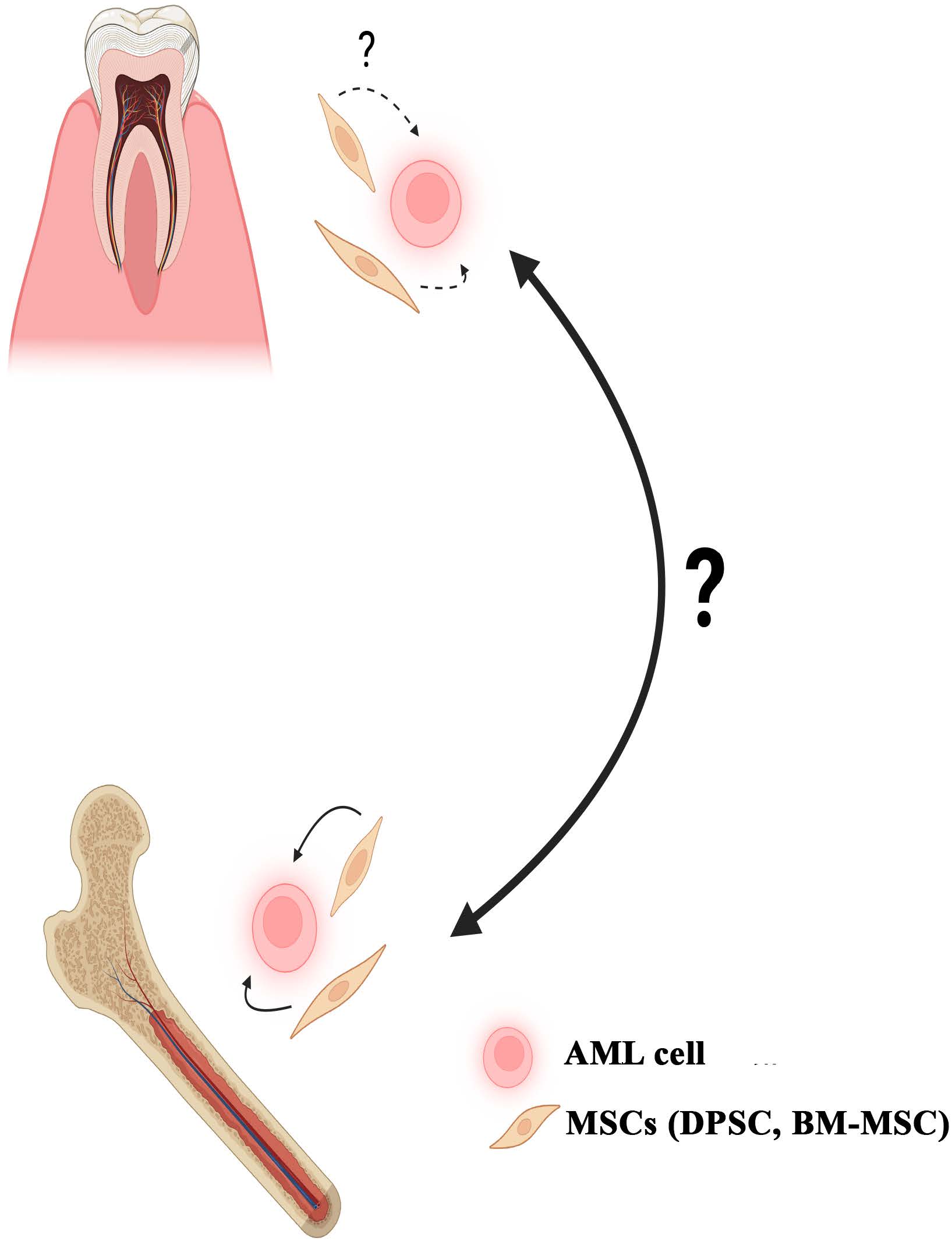
Parallel Stem Cell Niche in Bone Marrow and Oral Cavity – Key to Extramedullary Hematopoiesis and Support of Hematological Malignancies on Oral Tissues
DOI:
https://doi.org/10.13052/ijts2246-8765.2024.034Keywords:
Stem cells, dental pulp, bone marrow, hematopoiesis, hematological malignancy, oral cavity, cancerAbstract
This review article addresses an area of the literature with unanswered questions; although relevant to future treatment of leukemias. The literature describes bone marrow stromal microenvironment as support of leukemias. A key stromal support is mesenchymal stem cells (MSCs), which are similar to those identified in oral tissues, including the dental pulp (DPSC). Hematopoiesis has been reported in oral tissues, although the described activity seems to be distinct from extramedullary hematopoiesis at other sites when there is bone marrow dysfunction such as myelofibrosis. Another parallel between the bone marrow and oral tissues is the survival of leukemia cells. This review describes cases in which the dentist diagnoses leukemia, in particular acute myeloid leukemia (AML). The literature showed AML and other hematological malignancies in gingiva, leaving the question of the source of leukemia. We propose that this question is relevant considering the similar stromal support in bone marrow and oral tissues. It is difficult to determine if current treatments can target leukemia in oral tissues. This article consists of information to argue for continued research in this field.
Downloads
References
Crane, G. M., E. Jeffery, and S. J. Morrison. 2017. Adult haematopoietic stem cell niches. Nat Rev Immunol 17: 573–590.
Mende, N., and E. Laurenti. 2021. Hematopoietic stem and progenitor cells outside the bone marrow: where, when, and why. Exp Hematol 104: 9–16.
Yoshikawa, T., T. Noshi, H. Mitsuno, K. Hattori, K. Ichijima, and Y. Takakura. 2001. Bone and soft tissue regeneration by bone marrow mesenchymal cells. Materials Sci Eng C 17: 19–26.
Kawaguchi, H., A. Hirachi, N. Hasegawa, T. Iwata, H. Hamaguchi, H. Shiba, T. Takata, Y. Kato, and H. Kurihara. 2004. Enhancement of periodontal tissue regeneration by transplantation of bone marrow mesenchymal stem cells. J Periodontol 75: 1281–1287.
Li, Z. Y., L. Chen, L. Liu, Y. F. Lin, S. W. Li, and W. D. Tian. 2007. Odontogenic potential of bone marrow mesenchymal stem cells. J Oral Maxillofac Surg 65: 494–500.
Ishizaka, R., K. Iohara, M. Murakami, O. Fukuta, and M. Nakashima. 2012. Regeneration of dental pulp following pulpectomy by fractionated stem/progenitor cells from bone marrow and adipose tissue. Biomaterials 33: 2109–2118.
Kawaguchi, H., A. Hirachi, N. Hasegawa, T. Iwata, H. Hamaguchi, H. Shiba, T. Takata, Y. Kato, and H. Kurihara. 2004. Enhancement of periodontal tissue regeneration by transplantation of bone marrow mesenchymal stem cells. J Periodontol 75: 1281–1287.
Wilson, K. R., I.-H. Kang, U. Baliga, Y. Xiong, S. Chatterjee, E. Moore, B. Parthiban, K. Thyagarajan, J. L. Borke, and S. Mehrotra. 2018. Hematopoietic stem cells as a novel source of dental tissue cells. Sci Reports 8: 8026.
Krishnan, S., K. Wemyss, I. E. Prise, F. A. McClure, C. O’boyle, H. M. Bridgeman, T. N. Shaw, J. R. Grainger, and J. E. Konkel. 2021. Hematopoietic stem and progenitor cells are present in healthy gingiva tissue. J Exp Med 5: 218.
Hajishengallis, G., and J. M. Korostoff. 2017. Revisiting the Page & Schroeder model: the good, the bad and the unknowns in the periodontal host response 40 years later. Periodontol 2000 75: 116–151.
Kimura, Y., M. Komaki, K. Iwasaki, M. Sata, Y. Izumi, and I. Morita. 2014. Recruitment of bone marrow-derived cells to periodontal tissue defects. Frontiers Cell Dev Biol 2: 19.
Hattori, K., B. Heissig, and S. Rafii. 2003. The regulation of hematopoietic stem cell and progenitor mobilization by chemokine SDF-1. Leuk lymphoma 44: 575–582.
Mendt, M., and J. E. Cardier. 2015. Role of SDF-1 (CXCL12) in regulating hematopoietic stem and progenitor cells traffic into the liver during extramedullary hematopoiesis induced by G-CSF, AMD3100 and PHZ. Cytokine 76: 214–221.
Sherman, L. S., A. Condé-Green, O. A. Sandiford, and P. Rameshwar. 2015. A discussion on adult mesenchymal stem cells for drug delivery: pros and cons. Ther Deliv 6: 1335–1346.
Ehninger, A., and A. Trumpp. 2011. The bone marrow stem cell niche grows up: mesenchymal stem cells and macrophages move in. J Exp Med 208: 421–428.
Aqmasheh, S., P. Akbarzadehlaleh, D. P. Sarvar, and H. Timari. 2017. Effects of mesenchymal stem cell derivatives on hematopoiesis and hematopoietic stem cells. Adv Pharmaceutical Bulletin 7: 165.
Méndez-Ferrer, S., T. V. Michurina, F. Ferraro, A. R. Mazloom, B. D. MacArthur, S. A. Lira, D. T. Scadden, A. Ma’ayan, G. N. Enikolopov, and P. S. Frenette. 2010. Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature 466: 829–834.
Asada, N., Y. Kunisaki, H. Pierce, Z. Wang, N. F. Fernandez, A. Birbrair, A. Ma’ayan, and P. S. Frenette. 2017. Differential cytokine contributions of perivascular haematopoietic stem cell niches. Nature Cell Biol 19: 214–223.
Kunisaki, Y., I. Bruns, C. Scheiermann, J. Ahmed, S. Pinho, D. Zhang, T. Mizoguchi, Q. Wei, D. Lucas, and K. Ito. 2013. Arteriolar niches maintain haematopoietic stem cell quiescence. Nature 502: 637–643.
Eliasson, P., and J. I. Jönsson. 2010. The hematopoietic stem cell niche: low in oxygen but a nice place to be. J Cell Physiol 222: 17–22.
Kiel, M. J., Ö. H. Yilmaz, T. Iwashita, O. H. Yilmaz, C. Terhorst, and S. J. Morrison. 2005. SLAM family receptors distinguish hematopoietic stem and progenitor cells and reveal endothelial niches for stem cells. Cell 121: 1109–1121.
Parmar, K., P. Mauch, J.-A. Vergilio, R. Sackstein, and J. D. Down. 2007. Distribution of hematopoietic stem cells in the bone marrow according to regional hypoxia. Proc Natl Acad Sci 104: 5431–5436.
Winkler, I. G., N. A. Sims, A. R. Pettit, V. Barbier, B. Nowlan, F. Helwani, I. J. Poulton, N. van Rooijen, K. A. Alexander, and L. J. Raggatt. 2010. Bone marrow macrophages maintain hematopoietic stem cell (HSC) niches and their depletion mobilizes HSCs. Blood 116: 4815–4828.
Kusumbe, A. P., S. K. Ramasamy, and R. H. Adams. 2014. Coupling of angiogenesis and osteogenesis by a specific vessel subtype in bone. Nature 507: 323–328.
Nombela-Arrieta, C., G. Pivarnik, B. Winkel, K. J. Canty, B. Harley, J. E. Mahoney, S.-Y. Park, J. Lu, A. Protopopov, and L. E. Silberstein. 2013. Quantitative imaging of haematopoietic stem and progenitor cell localization and hypoxic status in the bone marrow microenvironment. Nature Cell Biol 15: 533–543.
Christodoulou, C., J. A. Spencer, S.-C. A. Yeh, R. Turcotte, K. D. Kokkaliaris, R. Panero, A. Ramos, G. Guo, N. Seyedhassantehrani, and T. V. Esipova. 2020. Live-animal imaging of native haematopoietic stem and progenitor cells. Nature 578: 278–283.
Kokkaliaris, K. D., L. Kunz, N. Cabezas-Wallscheid, C. Christodoulou, S. Renders, F. Camargo, A. Trumpp, D. T. Scadden, and T. Schroeder. 2020. Adult blood stem cell localization reflects the abundance of reported bone marrow niche cell types and their combinations. Blood 136: 2296–2307.
Kusumbe, A. P., S. K. Ramasamy, T. Itkin, M. A. Mäe, U. H. Langen, C. Betsholtz, T. Lapidot, and R. H. Adams. 2016. Age-dependent modulation of vascular niches for haematopoietic stem cells. Nature 532: 380–384.
Yamazaki, S., H. Ema, G. Karlsson, T. Yamaguchi, H. Miyoshi, S. Shioda, M. M. Taketo, S. Karlsson, A. Iwama, and H. Nakauchi. 2011. Nonmyelinating Schwann cells maintain hematopoietic stem cell hibernation in the bone marrow niche. Cell 147: 1146–1158.
Xu, J., Y. Wang, P. Guttorp, and J. L. Abkowitz. 2018. Visualizing hematopoiesis as a stochastic process. Blood Adv 2: 2637–2645.
Ding, L., T. L. Saunders, G. Enikolopov, and S. J. Morrison. 2012. Endothelial and perivascular cells maintain haematopoietic stem cells. Nature 481: 457–462.
Inra, C. N., B. O. Zhou, M. Acar, M. M. Murphy, J. Richardson, Z. Zhao, and S. J. Morrison. 2015. A perisinusoidal niche for extramedullary haematopoiesis in the spleen. Nature 527: 466–471.
Hosokawa, Y., I. Hosokawa, K. Ozaki, H. Nakae, K. Murakami, Y. Miyake, and T. Matsuo. 2005. CXCL12 and CXCR4 expression by human gingival fibroblasts in periodontal disease. Clin Exp Immunol 141: 467–474.
Ogawa, M., A. C. LaRue, and C. J. Drake. 2006. Hematopoietic origin of fibroblasts/myofibroblasts: Its pathophysiologic implications. Blood 108: 2893–2896.
Dzierzak, E., and N. A. Speck. 2008. Of lineage and legacy: the development of mammalian hematopoietic stem cells. Nature Immunol 9: 129–136.
Doulatov, S., F. Notta, E. Laurenti, and J. E. Dick. 2012. Hematopoiesis: a human perspective. Cell Stem Cell 10: 120–136.
Acar, M., K. S. Kocherlakota, M. M. Murphy, J. G. Peyer, H. Oguro, C. N. Inra, C. Jaiyeola, Z. Zhao, K. Luby-Phelps, and S. J. Morrison. 2015. Deep imaging of bone marrow shows non-dividing stem cells are mainly perisinusoidal. Nature 526: 126–130.
Kusumbe, A. P. 2016. Vascular niches for disseminated tumour cells in bone. J Bone Oncol 5: 112–116.
Saçma, M., J. Pospiech, R. Bogeska, W. de Back, J.-P. Mallm, V. Sakk, K. Soller, G. Marka, A. Vollmer, and R. Karns. 2019. Haematopoietic stem cells in perisinusoidal niches are protected from ageing. Nature Cell Biol 21: 1309–1320.
Zhang, J., Q. Wu, C. B. Johnson, G. Pham, J. M. Kinder, A. Olsson, A. Slaughter, M. May, B. Weinhaus, and A. D’Alessandro. 2021. In situ mapping identifies distinct vascular niches for myelopoiesis. Nature 590: 457–462.
Nanci, A. 2008. Enamel: composition, formation, and structure. Ten Cate’s Oral histology: Development, structure, and function. 183–184.
Gopal, S., K. P. Shetty, V. Jindal, and M. Saritha. 2011. Interrelationship of endodontic-Periodonctic-Periodontal lesions- an overview. Indian J Dental Sci 3.
Zhang, W., X. F. Walboomers, S. Shi, M. Fan, and J. A. Jansen. 2006. Multilineage Differentiation Potential of Stem Cells Derived from Human Dental Pulp after Cryopreservation. Tissue Eng 12: 2813–2823.
Gendron, R., D. Grenier, and L.-F. Maheu-Robert. 2000. The oral cavity as a reservoir of bacterial pathogens for focal infections. Microbes Inf 2: 897–906.
Silva, L. 2015. A literature review of inflammation and its relationship with the oral cavity. Global J Inf Dis Clin Res 1: 1–7.
Inönü, E., S. A. Kayis, M. A. Eskan, and S. S. Hakki. 2020. Salivary Del-1, IL-17, and LFA-1 levels in periodontal health and disease. J Periodontal Res 55: 511–518.
Giannopoulou, C., J. J. Kamma, and A. Mombelli. 2003. Effect of inflammation, smoking and stress on gingival crevicular fluid cytokine level. J Clin Periodontol 30: 145–153.
Hirose, M., K. Ishihara, A. Saito, T. Nakagawa, S. Yamada, and K. Okuda. 2001. Expression of Cytokines and Inducible Nitric Oxide Synthase in Inflamed Gingival Tissue. J Periodontol 72: 590–597.
McGee, J. M., M. A. Tucci, T. P. Edmundson, C. L. Serio, and R. B. Johnson. 1998. The Relationship Between Concentrations of Proinflammatory Cytokines Within Gingiva and the Adjacent Sulcular Depth. J Periodontol 69: 865–871.
Belstrøm, D., C. Damgaard, E. Könönen, M. Gürsoy, P. Holmstrup, and U. K. Gürsoy. 2017. Salivary cytokine levels in early gingival inflammation. J Oral Microbiol 9: 1364101.
Górska, R., H. Gregorek, J. Kowalski, A. Laskus-Perendyk, M. Syczewska, and K. Madaliñski. 2003. Relationship between clinical parameters and cytokine profiles in inflamed gingival tissue and serum samples from patients with chronic periodontitis. J Clin Periodontol 30: 1046–1052.
Sison, E. A., and P. Brown. 2011. The bone marrow microenvironment and leukemia: biology and therapeutic targeting. Expert Rev Hematol 4: 271–283.
Hasan, S., N. I. Khan, and L. B. Reddy. 2015. Leukemic gingival enlargement: Report of a rare case with review of literature. Int J Appl Basic Med Res 5: 65–67.
Cammarata-Scalisi, F., K. Girardi, L. Strocchio, P. Merli, A. Garret-Bernardin, A. Galeotti, F. Magliarditi, A. Inserra, and M. Callea. 2020. Oral Manifestations and Complications in Childhood Acute Myeloid Leukemia. Cancers (Basel) 12: 1634.
McCarthy, F. P., and P. H. Karcher. 1946. The Oral Lesions of Monocytic Leukemia. New Engl J Med 234: 787–790.
Menezes, L., and J. R. Rao. 2012. Acute myelomonocytic leukemia presenting with gingival enlargement as the only clinical manifestation. J Indian Soc Periodontol 16: 597–601.
Sheikh, O., and M. Perry. 2021. The Lips, Mouth, Tongue and Teeth: Part II. Diseases and Injuries to the Head, Face and Neck: A Guide to Diagnosis and Management 1085–1168.
Zhang, X., Y. Li, Z. Ge, H. Zhao, L. Miao, and Y. Pan. 2020. The dimension and morphology of alveolar bone at maxillary anterior teeth in periodontitis: a retrospective analysis-using CBCT. Intl J Oral Sci 12: 4.
Marchese, A., and J. L. Benovic. 2001. Agonist-promoted ubiquitination of the G protein-coupled receptor CXCR4 mediates lysosomal sorting. J Biol Chem 276: 45509–45512.
Arya, M., H. Ahmed, N. Silhi, M. Williamson, and H. R. Patel. 2007. Clinical importance and therapeutic implications of the pivotal CXCL12-CXCR4 (chemokine ligand-receptor) interaction in cancer cell migration. Tumor Bio 28: 123–131.
Kim, Y.-R., and K.-S. Eom. 2014. Simultaneous inhibition of CXCR4 and VLA-4 exhibits combinatorial effect in overcoming stroma-mediated chemotherapy resistance in mantle cell lymphoma cells. Immune Network 14: 296–306.
Burger, J. A., A. Spoo, A. Dwenger, M. Burger, and D. Behringer. 2003. CXCR4 chemokine receptors (CD184) and α
β
integrins mediate spontaneous migration of human CD34+ progenitors and acute myeloid leukaemia cells beneath marrow stromal cells (pseudoemperipolesis). Br J Haematol 122: 579–589.
Hial, H., Y. Nishi, T. Mlyazawa, Y. Matsudalra, Y. Matsudalra, and Y. Nishizuka. 1981. Mouse lymphoid leukemias: symbiotic complexes of neoplastic lymphocytes and their microenvironments. J Natl Cancer Inst 66: 713–722.
de Lourdes Perim, A., M. K. Amarante, R. L. Guembarovski, C. E. C. de Oliveira, and M. A. E. Watanabe. 2015. CXCL12/CXCR4 axis in the pathogenesis of acute lymphoblastic leukemia (ALL): a possible therapeutic target. Cell Mol Life Sci 72: 1715–1723.
Sison, E. A. R., and P. Brown. 2011. The bone marrow microenvironment and leukemia: biology and therapeutic targeting. Expert Rev Hematol 4: 271–283.
Allon, I., A. Pessing, I. Kaplan, D. M. Allon, and A. Hirshberg. 2014. Metastatic Tumors to the Gingiva and the Presence of Teeth as a Contributing Factor: A Literature Analysis. J Periodontol 85: 132–139.
Bann AlHazmi, B. 2021. Leukemia and periodontal health. J Pakistan Dental Assoc 30(01).
Costa, N. L., M. C. Valadares, P. P. C. Souza, E. F. Mendonça, J. C. Oliveira, T. A. Silva, and A. C. Batista. 2013. Tumor-associated macrophages and the profile of inflammatory cytokines in oral squamous cell carcinoma. Oral Oncol 49: 216–223.
Ramesh, R., and A. Sadasivan. 2017. Oral squamous cell carcinoma masquerading as gingival overgrowth. Eur J Dent 11: 390–394.
Bharanidharan, R., T. Dineshkumar, K. Raghavendhar, and A. R. Kumar. 2015. Squamous cell carcinoma of the gingiva: A diagnostic enigma. J Oral Maxillofac Pathol 19: 267.
Seow, W. K. 1994. Root agenesis associated with chronic infection and traumatic curettage of the maxillary sinus. Pediatr Dent 16: 227.
Pour, M. H. 2008. Malignant melanoma of the oral cavity: a review of literature. Indian Journal of Dental Research 19: 47–51.
de Andrade, B. A., R. B. Farneze, M. Agostini, E. B. Cortezzi, A. C. Abrahão, M. G. Cabral, A. Rumayor, and M. J. Romañach. 2017. Myeloid sarcoma of the oral cavity: A case report and review of 89 cases from the literature. J Clin Exp Dent 9: e1167–e1171.
Fernandes, K. S., M. Gallottini, T. Castro, M. F. Amato, J. S. Lago, and P. H. Braz-Silva. 2018. Gingival leukemic infiltration as the first manifestation of acute myeloid leukemia. Special Care in Dentistry 38: 160–162.
Dantas, R. C. M., V. D. C. Vieira, W. S. MagalhÃEs, M. S. Assis, T. F. L. D. E. Oliveira, V. A. Sarmento, and P. Leite-Ribeiro. 2020. Acte myeloid leukemia with initial manifestation in gingiva: A case report. Oral Surgery, Oral Medicine, Oral Pathol Oral Radiol 130: e219.